Category: Urinary
-

Structured Urinary Continence Assessment and Management Plan
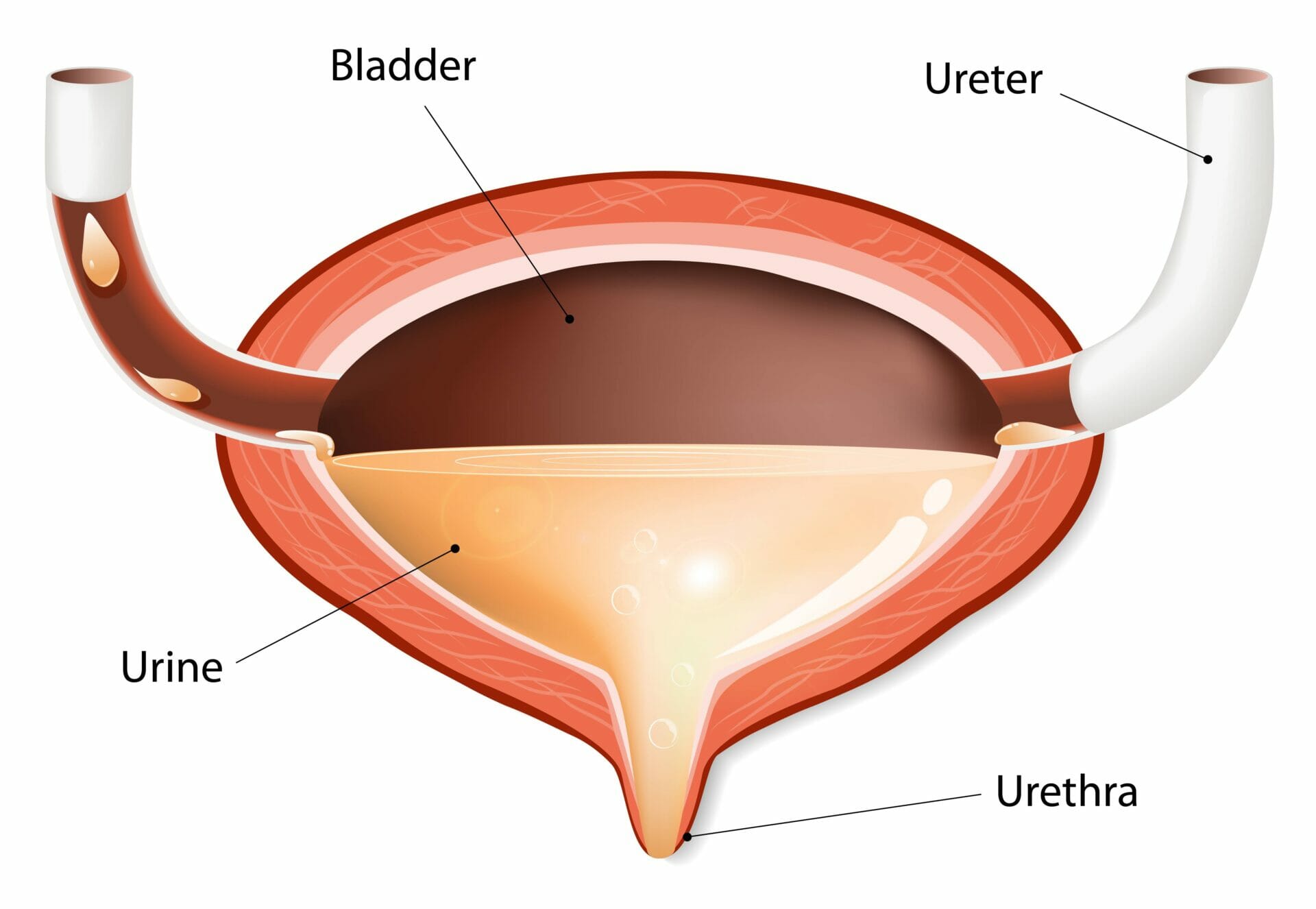
Urinary incontinence can have a significant impact on your quality of life. It can cause embarrassment and isolation, limit your ability to engage in social activities and increase the risk of falls and infections. That’s why it’s essential to have a structured urinary continence assessment and management plan to help you manage your symptoms effectively.…
-
Neurogenic bladder management
A neurogenic bladder is a condition where the nerve signals between the brain and the bladder are not working properly. This can happen due to damage to the nerves that control the bladder or other neurological conditions such as spinal cord injury, multiple sclerosis, or Parkinson’s disease. (Nitti & Singh, 2017; Rauch, Jhaveri, & Schurch,…