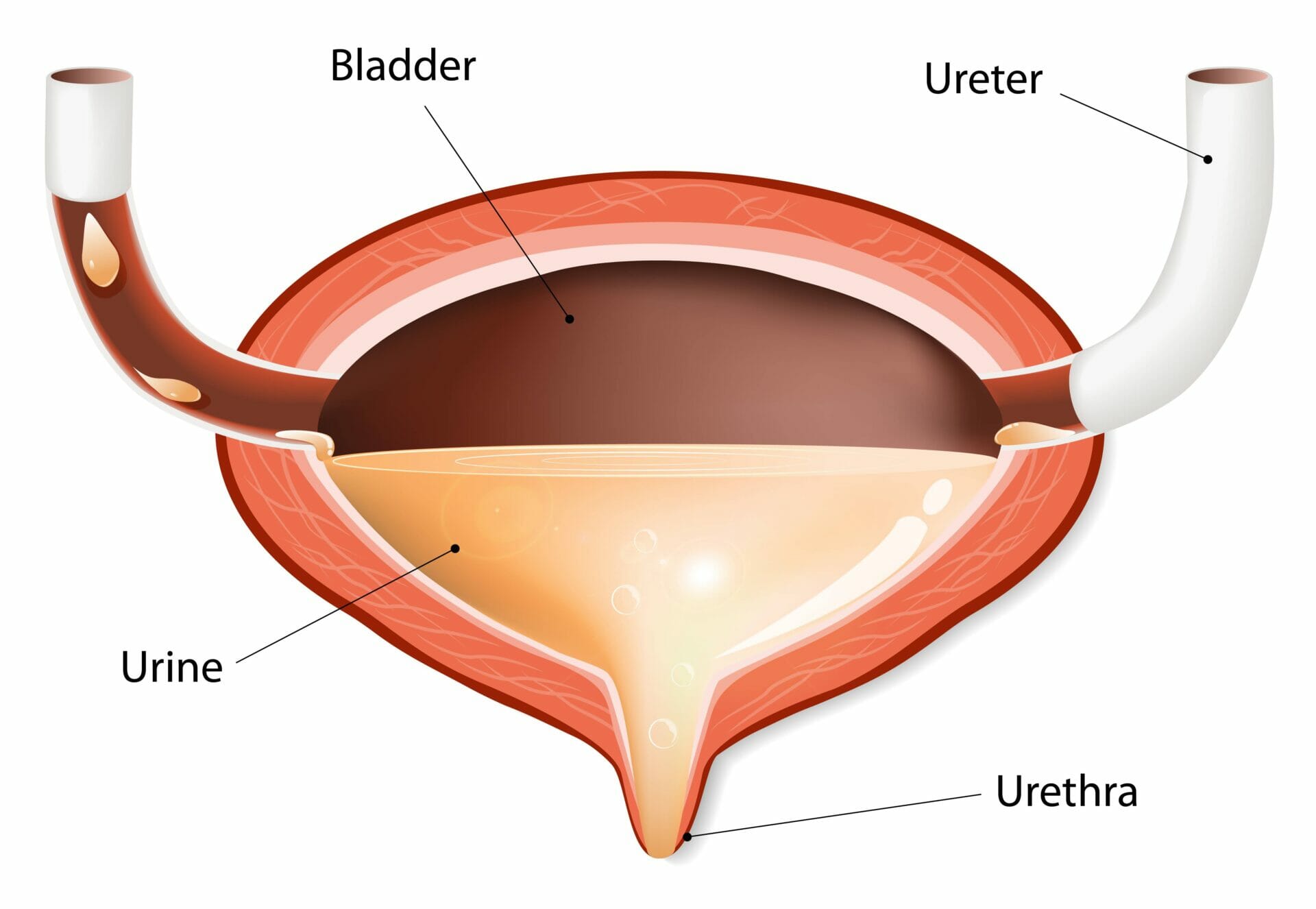
A neurogenic bladder is a condition where the nerve signals between the brain and the bladder are not working properly. This can happen due to damage to the nerves that control the bladder or other neurological conditions such as spinal cord injury, multiple sclerosis, or Parkinson’s disease. (Nitti & Singh, 2017; Rauch, Jhaveri, & Schurch, 2018). In this article, we will look at the various treatment options available for neurogenic bladder.
When you have a neurogenic bladder, you may experience issues such as difficulty emptying your bladder, incontinence (leaking urine), or even damage to your kidneys. These issues can affect your physical and mental well-being, making it difficult to carry out daily activities and potentially leading to feelings of embarrassment and low self-esteem. Furthermore, it can impair your skin’s intergrity.
Development of a Bladder Management Plan
To prevent incontinence, control your bladder function, avoid skin breakdown and maintain kidney health, it is important to establish a bladder management program. This program is based on your diagnosis as well as tests and assessments. Your healthcare professional may recommend yearly urodynamic testing to assess the bladder for changes or may have the test performed less frequently based on your clinical picture. (Gupta, DiGiovanni, & Park, 2017)
Treatment for neurogenic bladder may include strict following of the bowel management plan, catheterisation, medication, surgery and absorbent products.
Strict adherence to the bowel management program
Stool impaction, or the buildup of hard, dry feces in the rectum and colon, can affect your bladder function in a few ways. When stool becomes impacted, it can put pressure on the muscles and nerves that control the bladder, leading to problems with urinary function. Some common symptoms of stool impaction include difficulty passing stool, constipation, abdominal pain, and difficulty emptying the bladder completely (American College of Gastroenterology, 2019).
One way that stool impaction can affect your bladder function is by causing an obstruction in the rectum or colon. This can make it difficult for the bladder to empty completely, leading to urinary retention (National Institute of Diabetes and Digestive and Kidney Diseases, 2021). This can lead to feelings of discomfort, pressure in the bladder, incontinence and urinary tract infections.
Another way that stool impaction can affect your bladder function is by irritating the nerves that control the bladder. When the nerves become irritated, they can send signals to the brain that cause the bladder to contract even when it is not full (American College of Gastroenterology, 2019). This can lead to frequent urination and urgency.
Treatment for stool impaction typically involves manual removal of the impacted stool, often done by a healthcare professional. Laxatives or enemas may also be used to soften the stool and make it easier to pass (National Institute of Diabetes and Digestive and Kidney Diseases, 2021). In addition, increasing fluid and fiber intake and engaging in regular physical activity can help prevent future episodes of impaction (American College of Gastroenterology, 2019). If the impaction is caused by underlying medical conditions, such as neurological disorders, treatment of the underlying condition may be necessary.
Clean Intermittent Catheterisation (CIC)
You may be required to use intermittent catheterisation as a way to manage your bladder function. This is a common method for those with neurogenic bladders, particularly those who have some control over their hands and arms and it allows you to maintain your independence. (American Urological Association, n.d.)
The process of intermittent catheterisation involves inserting a catheter into your bladder to remove urine and it should be done using a clean technique. This means that you or the support worker assisting you must wash their hands thoroughly immediately before catheter entry and after the procedure is completed. (American Urological Association, n.d.)
You will likely be instructed to catheterise on a schedule of every four to six hours and to monitor your fluid intake. This will help to ensure that your bladder is being drained properly and that you are not experiencing any problems related to urinary retention. (National Institute of Diabetes and Digestive and Kidney Diseases, 2021)
There are a variety of catheters that can be used in this procedure. The most common type is the basic catheter, which can be lubricated by you or the person assisting you. Other types of catheters that may be used depending on specialised needs include pre-lubricated, hydrophilic (lubricant activated with sterile water), antibacterial, coudé tip for males with enlarged prostate glands and short catheters for women. Most catheters are single use, which means that they are intended for one-time use and should be discarded after use. (American Urological Association, n.d.)
Management of Autonomic Dysreflexia
If you have autonomic dysreflexia (AD) as a concern, there are several options available to you. One option is a sphincterotomy, also known as sphincterectomy, which is a surgical procedure that involves the removal of a portion of the internal urinary sphincter muscle in men. The procedure is performed to relieve symptoms caused by an overactive bladder or a narrowed urethra and it allows bladder drainage continuously out of the bladder, avoiding the reflex response of autonomic dysreflexia. An external catheter is used to collect urine in a urinal bag.
According to a review of literature, sphincterectomy has been identified as an effective surgical procedure to treat autonomic dysreflexia in participants with spinal cord injury (Pansadoro et al., 2008).
In more severe cases of AD, a suprapubic catheter may be placed through a surgical opening just over the bladder through the abdominal wall for continuous drainage. This option is available for both men and women.
Mitrofanoff procedure
A Mitrofanoff procedure is another option if you have poor hand control or intermittent catheterisation is anatomically difficult. This procedure creates a connection from the top of the bladder through the navel using the appendix or a small piece of the bowel. A catheter is then inserted intermittently through the navel to the bladder for the removal of urine. This procedure is often used with children, women, or men with a retracted penis.
Medications used in the management of neurogenic bladder
To treat neurogenic bladder, your doctor may recommend a number of medications. One common class of medications used for reflexive bladders that have tone (spasticity) is anticholinergic medications (American Academy of Family Physicians, n.d.). These medications work by blocking the action of the neurotransmitter acetylcholine, which helps to relax the muscles of neurogenic detrusor overactivity and improve bladder control. Examples of anticholinergic medications include oxybutynin, tolterodine, solifenacin, and darifenacin. If one anticholinergic medication does not work well for you or causes bothersome side effects, your healthcare provider may recommend trying an alternative medication that may be better suited to your needs.Another class of medications that may be used to treat bladder issues is alpha-blockers (American Academy of Family Physicians, n.d.). These medications work by relaxing the muscles of the bladder and the urethra, which can help to improve bladder control and reduce symptoms such as frequent urination and difficulty starting urination. Examples of alpha-blockers include tamsulosin and alfuzosin.
In some cases, your healthcare provider may recommend botulinum toxin (BOTOX) injections to calm a reflexive bladder (American Academy of Family Physicians, n.d.). These injections involve injecting small amounts of BOTOX into the bladder muscle, which helps to relax the muscle and improve bladder control. However, these injections need to be repeated on a regular schedule and also have some side effects such as urinary tract infection, and bladder or urinary retention.
Surgical Interventions in Neurogenic Bladder Dysfunction
There are a variety of surgical options to help improve your condition. One common surgical option for improving bladder control is a sphincterotomy (Nitti & Singh, 2017), which involves cutting a small portion of the muscle that surrounds the urethra to help relax the muscle and improve bladder control.
Another surgical option is suprapubic catheter placement (Sultan & Chancellor, 2017), which involves inserting a tube through the lower abdomen into the bladder to help drain urine. The Mitrofanoff procedure (Fader et al., 2018) is also an option, which involves creating a new way for the person to empty their bladder. This procedure involves making a small opening in the stomach and connecting it to the bladder, allowing the person to use a catheter to empty the bladder.
Bladder augmentation (Hussein et al., 2018) is another surgical option that can be performed to increase the size and bladder capacity. This procedure involves using tissue from other parts of the body to create a larger bladder.
Other surgical interventions include stents to open the urethra or ureters, urinary diversions, and ostomies. These options should be considered only if procedures that mimic natural bladder functioning are challenging.
Nerve transfers in the cauda equina (Salvatori & Gazzeri, 2017) are being performed to increase and enhance bladder, bowel, and sexual function in men and bladder and bowel function in women. As the nerves in the cauda equina are peripheral nerves, these nerves can be rerouted, transferred, and grafted to enhance bladder function.
For some individuals with cerebral palsy, a dorsal rhizotomy (Gupta et al., 2017) can be performed to reduce the number of nerve fibers (not the entire nerve) that increase tone (spasticity) to increase movement as well as bladder and bowel function.
Functional electrical stimulation procedures are also increasing options for individuals. Implanted and external electrodes (Rauch et al., 2018) are being used to increase bladder and bowel function.
Absorbent Products
Absorbent products such as undergarments, pads, panty shields, panty liners, and adult diapers can help prevent wetness and odors caused by neurogenic bladder. These products are designed to absorb urine and keep the skin dry, reducing the risk of skin irritation and infections. They come in various sizes and absorbencies, making it easy to find the right product for your needs. It is also important to change these products regularly, as they can become saturated and lose their effectiveness.
Bed pads can also be used to protect sheets and mattresses from wetness. These pads can be placed under the sheets and changed regularly to keep the bedding dry. This can be especially helpful for individuals who experience nighttime incontinence.
It is important to note that absorbent products are not a replacement for other forms of bladder management such as intermittent catheterisation, medications, or surgery, but they can provide added protection and improve quality of life. Consult with a healthcare provider to find the best solution for you.
Tips on Bladder Management
If you are experiencing issues with bladder function, it’s important to take care of your bladder to ensure proper functioning. One important tip for bladder care is to empty your bladder when you are upright or nearly upright. The effects of gravity can help empty urine from the bladder more effectively (Hussein et al., 2018).
Catheterisation is also an important aspect of bladder care. It is more efficient and complete when the catheter is withdrawn slowly to remove urine from the lower part of the bladder (Sultan & Chancellor, 2017). It’s important to wash your hands before the catheterisation set up and not to touch anything else, like wheels or clothes, prior to touching or inserting a catheter. This helps reduce the risk of infection (Fader et al., 2018).You should also clean the area around the urethra prior to inserting a catheter, and lubricate a catheter thoroughly prior to insertion. This helps reduce discomfort and also reduce the risk of infection (Nitti & Singh, 2017).
Another important aspect of bladder care is to drink water according to your bladder management plan (Gupta et al., 2017). Avoid drinks high in sugar, caffeine, and sugar substitute as they can increase the amount of urine produced rapidly.
Moving your legs can also help stimulate muscle movement in the abdomen, which can help stimulate function in the bladder, bowel, and muscles of your legs, and reduce edema (Salvatori & Gazzeri, 2017). Practicing excellent hygiene can also help avoid urinary tract infections (Rauch et al., 2018)
.
Lastly, maintaining your bowel program is also important for overall bladder health and functioning (Hussein et al., 2018).
Conclusion
Neurogenic bladder management is an important part of healthcare for those with neurological conditions. It involves the use of medications, lifestyle changes, and other treatments to help manage bladder control issues. While there are many different approaches to neurogenic bladder management, it is important to understand that each individual’s needs will be unique and require a tailored approach.
The first step in managing a neurogenic bladder condition is understanding the underlying cause of the issue. This can range from spinal cord injuries or diseases like multiple sclerosis or Parkinson’s disease, all of which can affect how your body controls its urinary system. Once you know what has caused your condition, you can work with your doctor on finding an appropriate treatment plan that works best for you and meets your specific needs.
Medications are often used as part of a comprehensive treatment plan for neurogenic bladders; they may include anticholinergics (to reduce muscle spasms), alpha blockers (to relax muscles), or even opioids (for pain relief). Surgery may also be recommended depending on the severity and type of symptoms experienced by patients with this condition. Additionally, lifestyle modifications such as avoiding caffeine-containing beverages or drinking plenty fluids throughout the day may help improve symptoms associated with this disorder over time too!
It’s also essential to remember that self-care plays an integral role in successful neurogenic bladder management plans too! For example: practicing good hygiene habits like wiping front-to-back after using the restroom; wearing loose clothing made from breathable fabrics; scheduling regular bathroom breaks throughout each day; setting reminders if needed – these are all great ways to ensure proper care when dealing with this particular medical issue!
IManaging a neurogenic bladder requires patience and dedication but it doesn’t have to be overwhelming either! With careful planning and support from family members/friends/doctors alike – anyone living with this disorder should feel empowered enough take charge over their own health journey while still feeling supported every step along way too!