Category: Diabetes
-
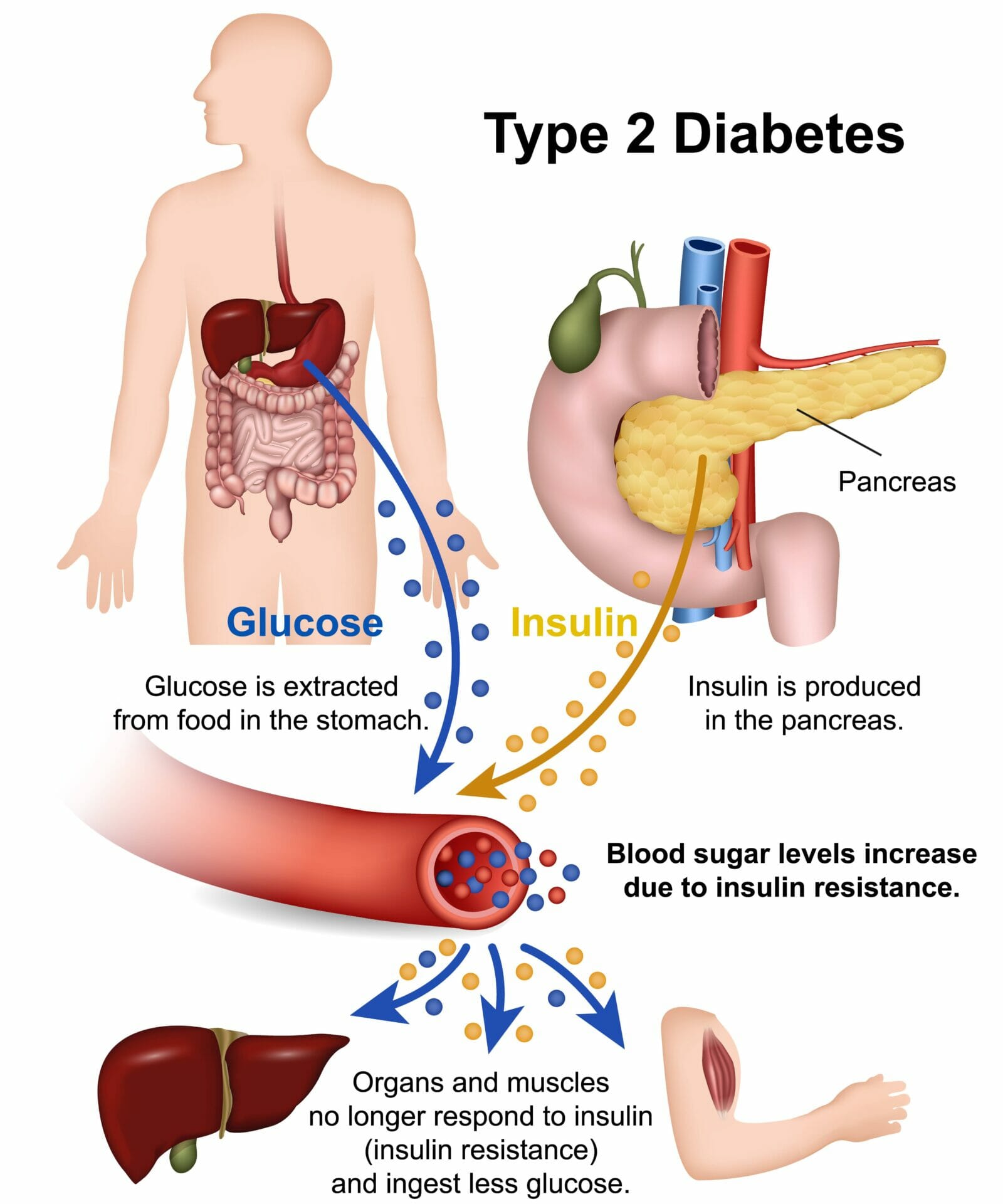
What causes Type 2 diabetes?
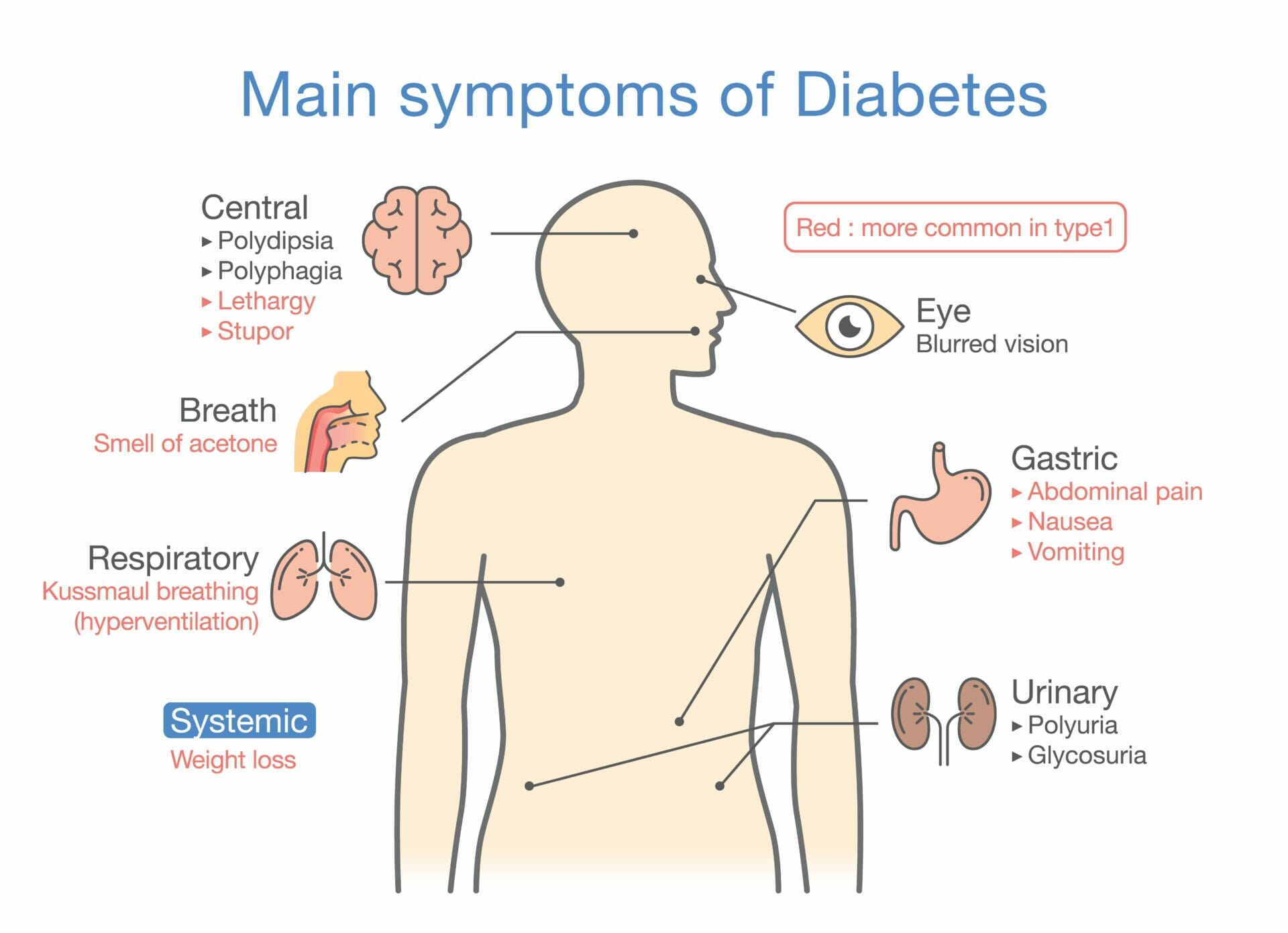
Type 2 diabetes is a chronic condition characterised by high blood sugar levels. It occurs when the body becomes resistant to the effects of insulin or fails to produce enough insulin to regulate blood sugar properly. Insulin is a hormone that helps move glucose from the bloodstream into cells for energy. Table of contents: What…
-

Understanding glycated haemoglobin (hba1c test) – a key indicator of diabetes control
Glycated Haemoglobin (HbA1c) is a crucial indicator used to measure the average blood glucose levels over a period of two to three months. It provides valuable insights into a person’s diabetes control and helps healthcare professionals in assessing the effectiveness of treatment plans. HbA1c is formed when glucose in the blood combines with haemoglobin, the…
-

Types of insulin for diabetes
Insulin is a hormone that plays a crucial role in regulating blood sugar levels in the body. It is produced by the pancreas, specifically by the beta cells in the Islets of Langerhans. Insulin allows the cells in the body to use glucose from the bloodstream as a source of energy. Without insulin, the body…
-

Exploring the different types of diabetic neuropathy and their impact on daily life
Diabetic neuropathy: a common complication of diabetes that affects the nerves, leading to various symptoms and complications. It is estimated that around 50% of people living with diabetes develop some form of neuropathy during their lifetime. Table of contents: Exploring the different types of diabetic neuropathy and their impact on daily life Causes and Risk…
-
Do You Know The 4Ts of Type 1 Diabetes
Understanding the basics of Type 1 Diabetes Type 1 diabetes is a chronic autoimmune condition that affects millions of people worldwide. It occurs when the immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas, known as beta cells. Without insulin, a hormone that helps regulate blood sugar levels, the body is unable…
-

Calibration of a glucometer
If you are living with diabetes, then it is important to keep your blood sugar levels in check. One of the most effective ways to do this is by using a glucometer. However, for accurate readings and reliable results, it is essential that you calibrate your glucometer regularly. In this blog article we will discuss…
-

Foot care and diabetes
As someone living with diabetes, it’s essential to prioritise footcare to prevent serious complications such as nerve damage, kidney disease, and eye problems. High blood sugar levels can damage the nerves and blood vessels in the feet, leading to a loss of feeling and circulation. This can make it difficult to detect injuries and infections,…